Diabetes


Diabetes Care & AHC Diabetes Package
Your Guide to Early Detection, Management, and Comprehensive Care
For Patients Who May Not Realize They Have Diabetes
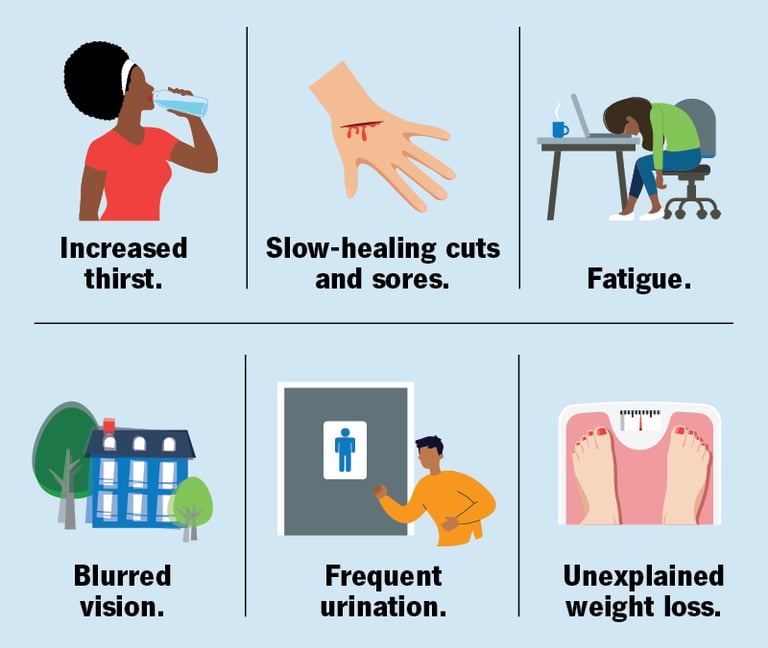
1. What are the common symptoms of undiagnosed diabetes?
Early signs include
frequent urination
excessive thirst
unexplained weight loss
constant fatigue
blurred vision
slow-healing wound
tingling/numbness in hands or feet.
If you experience these symptoms, book a diagnostic test with AHC to rule out diabetes.
2. Who is at risk of developing diabetes?
Risk factors include:
Family history of diabetes
Being overweight or obese
Sedentary lifestyle
High blood pressure or cholesterol
History of gestational diabetes
Age over 45
3. I feel fine. Should I still get tested?
Yes! Diabetes can be “silent” for years. AHC recommends routine screenings for high-risk individuals. Our Diabetes Package includes regular blood tests to catch issues early.
4. How does AHC help if I’m diagnosed with diabetes?
We provide a personalized care plan with:
Diagnostics: Regular blood sugar, kidney, and cholesterol monitoring.
Expert consultations: Doctors, dietitians, and specialists to guide you.
Preventive care: Tools to avoid complications like nerve damage or heart disease.
For Patients to Manage Diabetes Well
1. How can I stay on track with my diabetes management?
AHC’s Diabetes Package supports your success with:
Regular check-ups: HbA1c tests, kidney function, and cholesterol panels.
Tailored medications/supplements: Updated based on your progress.
Nutritional guidance: Dieticians create meal plans to stabilize blood sugar.
Muscle stimulation therapy: For diabetic neuropathy pain relief.
2. Why are kidney and cholesterol checks important?
Diabetes increases cardiovascular and kidney risks. Our package includes annual kidney function tests (eGFR, urine albumin) and lipid profiles to safeguard your heart and organs.
3. Can I reverse diabetes complications?
While diabetes is chronic, early action prevents worsening. For neuropathy (nerve damage), AHC offers muscle stimulation therapy to improve circulation and reduce pain.
4. How often should I consult my care team?
We recommend:
Quarterly doctor visits for medication reviews.
Bi-annual dietitian sessions to refine your nutrition plan.
Annual neuropathy/cardiovascular screenings.
About the AHC Diabetes Package
1. What’s included in the package?
Diagnostics: Blood sugar, kidney, and cholesterol tests.
Treatment: Best-in-class medicines, supplements, and neuropathy therapies.
Consultations: Doctors, dietitians, and nutritionists.
Preventive care: Personalized plans for long-term health.
2. How does this package improve my care?
By bundling services, we ensure consistent monitoring, early problem detection, and holistic support—reducing hospitalizations and complications.
3. How do I enroll?
Visit or call to schedule your first assessment.
Take Charge of Your Health Today!
Whether you’re newly diagnosed or managing diabetes well, the AHC Diabetes Package empowers you to live healthier.
📞 Contact Us: 800 748 0044
📍 Visit:
AHC-OPD : Kalyani Nagar, Pune
Early detection saves lives. Proactive care ensures longevity.


Diabetes Package
Relationship Manager for regular follow-ups and checks. Just like your gym trainer but more like a 'buddy'
Regular monitoring and trends
Dietician and Nutritionist plans
Diagnostics
Diabetes daily Medicines 3 in 1 for Diabetes Management and Kidney protection
Diabetes support supplements Vit D3, COQ 10 and Vit B12
Optional Neuropathy medicine
Procedures (Nerve Health)
Transcutaneous Electrical Nerve Stimulation 2-4 weeks, each session is worth 2000 and for 30 mins.
Muscle simulators to prevent muscle dystrophy and diabetic neuropathy management
Doctors Consultations
Monthly :
Quarterly :
Yearly :
1. The Intertwined Relationship Between Hypertension, Diabetes, and Kidney Disease
How diabetes damages kidneys: Over time, high blood sugar (hyperglycemia) can damage the small blood vessels in the kidneys, which are responsible for filtering waste from the blood. This damage, known as diabetic nephropathy, leads to scarring and a gradual decline in kidney function.
How hypertension damages kidneys: High blood pressure puts extra strain on the blood vessels in the kidneys, leading to damage and a decline in their filtering ability. This can create a vicious cycle, as damaged kidneys are less able to regulate blood pressure, which in turn causes more kidney damage.
A synergistic effect: When a patient has both diabetes and hypertension, the risk of developing CKD is significantly higher, and the progression of the disease is often more rapid.
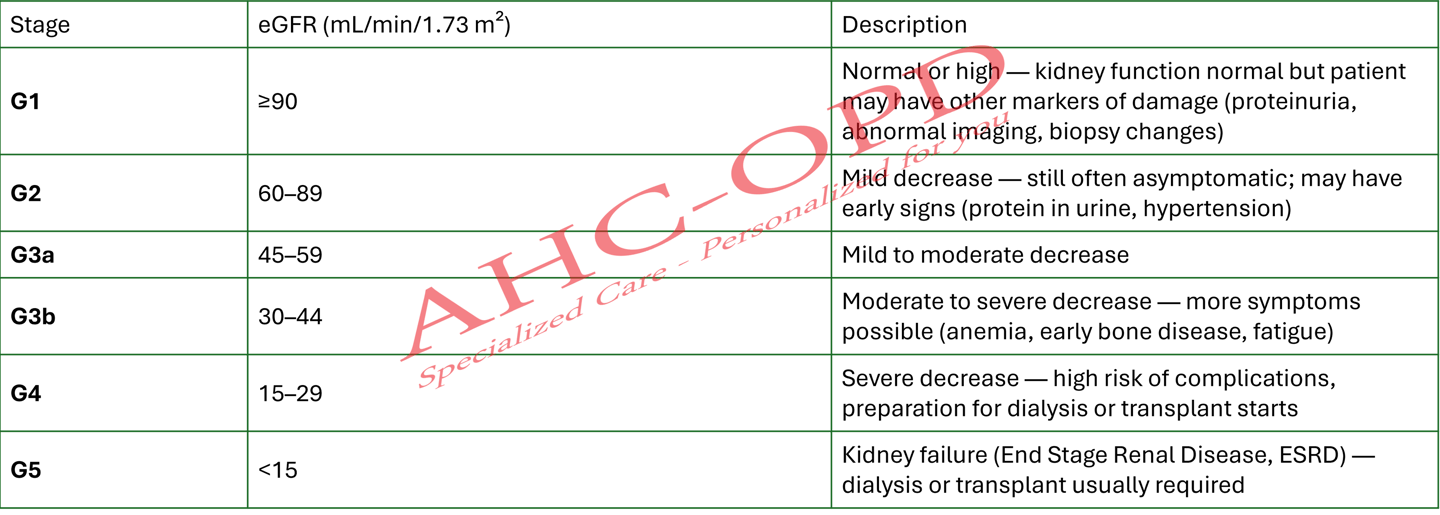
2. Stages of Chronic Kidney Disease (CKD)
CKD is a progressive condition categorized into five stages based on the estimated glomerular filtration rate (eGFR) and albuminuria (protein in the urine). The eGFR is a measure of how well the kidneys are filtering waste, and a normal eGFR is typically 90 mL/min/1.73 m2 or higher.
Stage 1: eGFR of 90 or greater. The kidneys are functioning normally, but there are signs of kidney damage, such as a small amount of protein in the urine (albuminuria). There are usually no symptoms.
Stage 2: eGFR between 60 and 89. Mild kidney damage is present, and the eGFR has started to decline. As with Stage 1, symptoms are often absent.
Stage 3: eGFR between 30 and 59. This stage indicates mild to moderate kidney damage. Patients may start to experience symptoms like fatigue, swelling in the hands and feet, and high blood pressure. This stage is further divided into 3a (eGFR 45-59) and 3b (eGFR 30-44).
Stage 4: eGFR between 15 and 29. This is severe kidney damage, and symptoms are more pronounced. It is the last stage before kidney failure, and a patient will likely be planning for treatment options like dialysis or a kidney transplant.
Stage 5: eGFR less than 15. The kidneys are nearing or have reached complete failure. At this point, waste products build up in the body, and patients require dialysis or a kidney transplant to survive.
3. Medications and Their Impact on Renal Function
It's crucial to be aware of the medications that can both protect and potentially harm the kidneys, especially in hypertensive and diabetic patients.
Renoprotective Medications: Certain drugs are specifically prescribed to slow the progression of kidney damage.
ACE inhibitors (e.g., lisinopril): These drugs block a substance that narrows blood vessels, helping to lower blood pressure and reduce pressure on the kidney filters. They are often a first-line treatment for patients with diabetes and CKD.
Angiotensin II Receptor Blockers (ARBs) (e.g., losartan): These drugs have a similar effect to ACE inhibitors and are used for patients who cannot tolerate ACE inhibitors.
SGLT2 inhibitors (e.g., canagliflozin, empagliflozin): Originally for diabetes, these newer drugs have shown significant benefits in slowing CKD progression and reducing cardiovascular risk.
GLP-1 receptor agonists (e.g., liraglutide, semaglutide): Also diabetes medications, they have a positive impact on both cardiovascular and kidney health.
Medications that can cause kidney problems: While necessary for pain and other conditions, certain over-the-counter and prescription drugs can be hard on the kidneys, especially with long-term use.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Long-term use of drugs like ibuprofen and naproxen can damage the kidneys. Patients with CKD should be advised to avoid them.
Proton Pump Inhibitors (PPIs): Some studies suggest a link between the long-term use of these heartburn medications (e.g., omeprazole, lansoprazole) and an increased risk of CKD.
4. Monitoring and Assessment
Regular monitoring is essential for early detection and management of kidney issues in these patients. Your protocols should include:
eGFR (Estimated Glomerular Filtration Rate): A blood test that estimates how much blood the kidneys filter per minute. It's a key indicator of kidney function.
UACR (Urine Albumin-to-Creatinine Ratio): A urine test that checks for albumin (a type of protein) in the urine. Even small amounts can be an early sign of kidney damage.
Blood Pressure Monitoring: Consistent and accurate blood pressure measurements are critical, as hypertension is a major driver of kidney damage.
HbA1c: For diabetic patients, monitoring HbA1c is essential to assess long-term blood sugar control, which directly impacts kidney health.
Electrolyte Levels: Monitoring potassium and other electrolytes is important, as kidney dysfunction can lead to imbalances. For example, some blood pressure medications (ACE inhibitors, ARBs) can increase potassium levels (hyperkalemia), which can be dangerous.
Kidney (Chronic Kidney Disease-CKD)
⚡ Creatine & Creatinine – Myths vs Facts
❌ Myth 1: “Creatine supplement increases creatinine, so it damages kidneys.”
✅ Fact:
Creatine monohydrate can slightly raise blood creatinine because some of it naturally breaks down into creatinine. But in healthy people with normal kidneys, this is not harmful. Doctors look at the overall picture (eGFR, urine tests) before deciding if the kidneys are truly affected.
❌ Myth 2: “Creatine monohydrate and creatinine are the same thing.”
✅ Fact:
No. Creatine is a nutrient that stores energy in muscles (like charging a battery). Creatinine is the waste product after creatine is used (like exhaust fumes). One builds energy, the other signals waste.
❌ Myth 3: “If my creatinine is high, I must stop eating protein and creatine completely.”
✅ Fact:
High blood creatinine usually means the kidneys are not filtering well, not that creatine from food is the cause. Your doctor may advise reducing excess protein supplements, but a balanced diet with normal protein is essential to maintain muscle and health.
❌ Myth 4: “Creatine supplements cause kidney failure.”
✅ Fact:
There is no strong scientific evidence that normal doses (3–5 g/day) of creatine monohydrate cause kidney failure in healthy people. But in patients who already have CKD, extra creatine is usually not advised because their kidneys cannot clear creatinine efficiently.
❌ Myth 5: “High creatinine always means dialysis.”
✅ Fact:
Not always. A slightly high creatinine can be due to dehydration, medications, or temporary stress on kidneys. Dialysis is considered only when kidney function is very low (eGFR <15) and symptoms appear.
🩺 Understanding Your Kidney Function Test (eGFR & Urine Albumin)
Your kidneys act like the body’s natural filters. They clean the blood, remove waste, and balance fluids. Two important tests are used to check how well your kidneys are working:
1️⃣ eGFR – Estimated Glomerular Filtration Rate
What it means: This number tells us how well your kidneys are filtering blood.
Normal: Above 90 (if no other kidney damage is seen).
Mildly low: 60–89 – may be normal in some people but needs monitoring if you have diabetes, high blood pressure, or other risks.
Moderately low: 30–59 – indicates kidney disease that needs medical care.
Severely low: 15–29 – serious kidney damage, often with symptoms.
Very low (<15): Kidney failure – dialysis or transplant is usually needed.
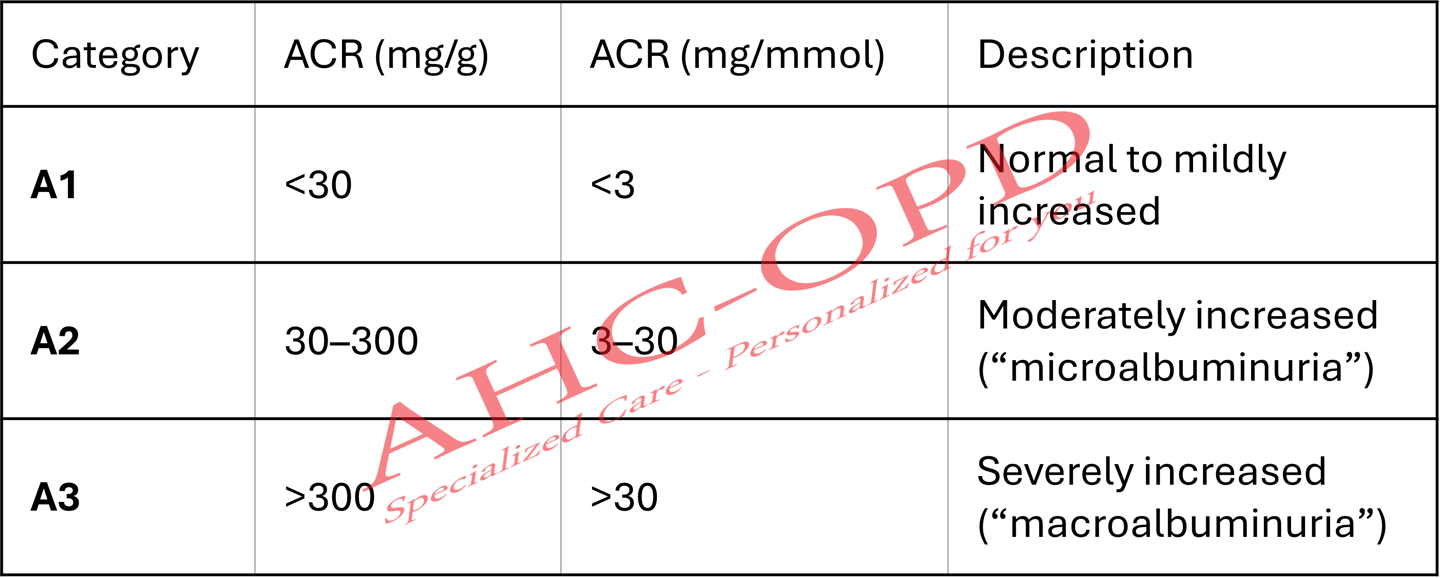
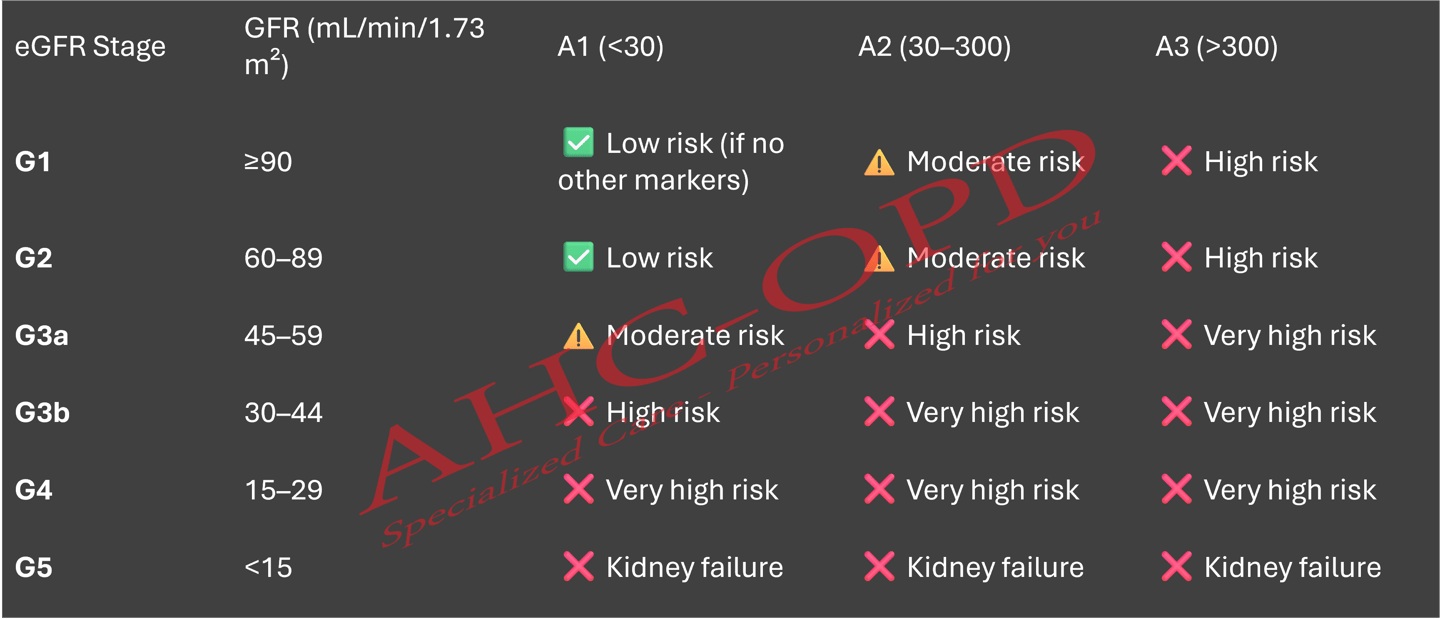
2️⃣ Urine Albumin (ACR – Albumin/Creatinine Ratio)
Albumin is a type of protein. Normally, the kidneys should not let protein leak into urine. If they do, it’s an early warning sign of kidney damage.
A1 (<30 mg/g): Normal to mildly increased – healthy kidneys.
A2 (30–300 mg/g): Moderately increased – “early leak,” kidneys under stress.
A3 (>300 mg/g): Severely increased – significant kidney damage.
3️⃣ Putting it Together – Kidney Health Grid
Doctors look at both eGFR and Urine Albumin to understand your kidney health:
Normal eGFR + No protein (A1) → Healthy kidneys.
Normal eGFR + Protein present (A2 or A3) → Early kidney damage, even if kidney strength looks fine.
Low eGFR (<60) → Chronic Kidney Disease (CKD). The lower the number, the more serious it is.
Low eGFR + High protein → Higher risk of kidney failure and heart problems, needs closer monitoring and treatment.
✅ Key Takeaways for Patients
A single low reading does not always mean permanent kidney disease. Tests may need to be repeated.
Diabetes, high blood pressure, obesity, and family history are the most common risk factors.
Lifestyle changes (controlling blood sugar, BP, avoiding excess salt, not overusing painkillers) can protect your kidneys.
Regular check-ups with your doctor can slow or prevent kidney damage.
❓ Kidney Function Test – Frequently Asked Questions (FAQ)
1. Does a low eGFR always mean kidney failure?
No. A single low eGFR does not always mean permanent damage. Sometimes it can be due to dehydration, recent illness, or lab variation. Your doctor may repeat the test to confirm.
2. Can kidneys recover if eGFR is low?
Yes, in some cases. If the low eGFR is due to temporary causes (like dehydration, infection, blockage, or medication side effects), kidney function may improve after treatment. But if it’s due to chronic kidney disease (CKD), the damage is usually permanent, though progression can be slowed.
3. If my eGFR is 60–89, is it dangerous?
Not always. Many people with an eGFR in this range have no symptoms. But if you also have diabetes, high blood pressure, or protein in urine, it means early kidney disease and needs monitoring.
4. At what eGFR do patients need dialysis?
Dialysis is usually considered when eGFR falls below 15 (Stage 5 CKD) and the patient develops symptoms such as swelling, nausea, breathlessness, or very high potassium levels. Not everyone with eGFR <15 starts dialysis immediately – the doctor decides based on overall health.
5. What is urine albumin and why is it important?
Albumin is a protein. If it leaks into urine, it’s an early warning sign of kidney stress or damage – often before eGFR becomes abnormal. Even a small leak (called microalbuminuria) is important to detect.
6. Can lifestyle changes improve kidney health?
Yes ✅. Controlling blood sugar, blood pressure, reducing salt intake, eating a balanced diet, exercising, avoiding smoking and excess painkillers can protect your kidneys and slow CKD progression.
7. I feel fine. Do I still need to worry about a low eGFR?
Yes. Kidney disease is often called a “silent disease” because it can progress without symptoms until very late. That’s why regular tests are important if you are at risk.
8. Should I see a kidney specialist (nephrologist)?
Yes, if your eGFR is <60 for 3 months or more.
Or if you have high urine protein (A2 or A3).
Or if you already have diabetes, high BP, or family history of kidney disease.
Hypertension
Pulse Pressure (PP) and Mean Arterial Pressure (MAP) are highly reliable and clinically significant markers for assessing cardiovascular health. While systolic (SBP) and diastolic (DBP) blood pressure readings are the cornerstone of hypertension diagnosis, PP and MAP provide deeper, more nuanced insights into the underlying hemodynamics and long-term risk. They are not just derived numbers; they are powerful indicators of vascular health and organ perfusion.
Pulse Pressure (PP)
Pulse Pressure is the difference between your systolic and diastolic blood pressure, calculated as PP = SBP - DBP. It represents the force the heart generates each time it contracts.
Reliability & Clinical Significance: PP is a crucial and reliable indicator of arterial stiffness and an independent predictor of cardiovascular risk, especially in individuals over the age of 50.
Wide Pulse Pressure (> 60 mmHg): This is a strong red flag 🚩. A wide PP suggests that major arteries, particularly the aorta, have lost their elasticity. This condition, known as arteriosclerosis, means the arteries can't properly buffer the force of blood being pumped from the heart. This leads to higher systolic pressure and lower diastolic pressure, widening the PP. A persistent wide PP is strongly linked to:
Increased risk of atrial fibrillation.
Higher likelihood of myocardial infarction (heart attack) and stroke.
Poorer outcomes in patients with heart failure.
Narrow Pulse Pressure (< 40 mmHg): A narrow PP can indicate a reduced stroke volume, which is the amount of blood pumped out of the left ventricle with each beat. This is often seen in conditions such as:
Congestive heart failure, where the heart's pumping ability is weakened.
Shock or significant blood loss (hemorrhage), leading to decreased cardiac output.
Aortic stenosis, a narrowing of the aortic valve that obstructs blood flow from the heart.
Mean Arterial Pressure (MAP)
Mean Arterial Pressure is the average arterial pressure throughout one complete cardiac cycle. It's considered a better indicator of organ perfusion than SBP alone. It is calculated as MAP = DBP + 1/3(SBP - DBP).
Reliability & Clinical Significance: MAP is an extremely reliable and critical measurement, particularly in acute and critical care settings. It reflects the driving pressure that ensures blood flow to vital organs.
High MAP (> 100 mmHg): A chronically elevated MAP means there is excessive pressure in the arteries. This sustained high pressure can:
Force the heart to work harder, leading to left ventricular hypertrophy (thickening of the heart muscle), a major risk factor for heart failure.
Damage the delicate endothelial lining of blood vessels, accelerating atherosclerosis (plaque buildup).
Increase the risk of aneurysm and stroke.
Low MAP (< 65 mmHg): This is a critical threshold. A MAP below this level is dangerous because it signifies that the pressure is insufficient to perfuse vital organs. This can lead to ischemia (inadequate oxygen supply) and organ damage. It is a defining parameter in managing:
Septic shock, where maintaining a MAP ≥ 65 mmHg is a primary treatment goal to prevent organ failure.
Trauma and major surgery to ensure adequate blood flow to the brain, kidneys, and heart.
Synthesis and Conclusion
While Systolic BP and Diastolic BP are essential for diagnosing hypertension, Pulse Pressure and Mean Arterial Pressure provide critical, complementary information.
PP offers a window into the structural health of the arteries (stiffness).
MAP provides a real-time assessment of perfusion pressure to vital organs.
